Preoccupation with aerosol-generating procedures broke dentistry
Patient care almost became secondary. Dentistry seemingly boxed themselves in as non-essential. Self-protection became the focus.
by KEVIN KUO DDS, MMSc | June 15, 2020
BEFORE COVID-19 - Aerosols long existed in dentistry before COVID-19 in 2020.
In fact, Dr. Richard Wilson Page developed the modern dental high-speed handpiece in the 1950s. Dentsply commercialized the first dental ultrasonic scalers around the same time period.
Dentists, since then, drilled on teeth over 100,000 RPMs, and dental hygienists scaled near the gingiva at 20,000 Hz or more.
Dental personnel and organizations had been aware of aerosols for decades and worked through them without consternation.
On a personal note, the word “aerosol” was only included a total of fifteen times in four years of dental school lectures, of approximately 700,000 words.
Similarly, the Journal of the American Dental Association (JADA)—the premier research journal in dentistry—only published around nine articles specifically referencing dental aerosols in the years 1964-2003.
Even the serious SARS pandemic in 2003-2004 triggered no perspective changes amongst the dental community. A 2004 JADA article published concerns over dental aerosols, with references to SARS, but created no increase in dental aerosol publications in the following years.
Dental aerosols were not well-studied due to overall indifference in dentistry.
A Google search further surmises this dental symbiotic relationship with aerosols. From the years 1998 (birth of Google) to 2019, no references for the term “dental aerosol generating procedures” resulted in the search engine. The phrase did not exist until March 2020.
DURING COVID-19 - Suddenly, dentistry only cared about dental aerosol-generating procedures (AGPs).
A screenshot of a New York Times interactive story.
On March 15th, 2020, a viral New York Times interactive story listed dentistry as one of the occupations most at risk of COVID-19. Dental personnel quickly shared this story around social media.
The CDC and OSHA likely created the movement in the “aerosol-generating procedure” syntax in dentistry. Both agencies indiscriminately migrated the terminology from medicine. For many years, AGPs were only referenced in medicine, regarding intubation, extubation, tracheostomy suctioning, invasive mechanical ventilation, and nebulized medicine.
The guidelines and recommendations from the American Dental Association (ADA) then further relayed the focus on dental aerosol-generating procedures.
Many state dental organizations, dental boards, and governments followed suit with an almost global recommendation for dental personnel to use N95s and other less typical PPE when conducting any dental aerosol-generating procedures.
At this point in March to the present in June, even without solid scientific evidence, the transmission of COVID-19 via dental aerosol-generating procedures has practically and controversially become an absolute fact in dentistry.
THE RESULT AFTER THE RISE OF DENTAL AGPs - Patient care almost became secondary. Dentistry seemingly boxed themselves in as non-essential. Self-protection became the focus.
In May 2020, as states begin to re-open, numerous dentists looked forward to re-opening to elective treatments due to significant financial burden from longterm partial closures as with any business during the COVID-19 pandemic.
However, the newfound obsession with AGPs sparked a race in dentistry to compile PPE mirroring medical personnel actively treating COVID-19 confirmed patients in hospitals. This preoccupation over PPE included N95s, KN95s, gowns, goggles, and more.
All-of-a-sudden, new non-traditional dental distributors selling PPE, gadgets, and air filters flooded the dental market. Even traditional dental distributors tried to sell unproven items.
Many dental practices haphazardly bought KN95 masks in bulk from upstart distributors—likely random individuals posing as legitimate dental distributors—without insuring the filtration quality. The NPPTL eventual determined that a significant proportion of imported KN95 masks filtered much less than 95% of small micron particles.

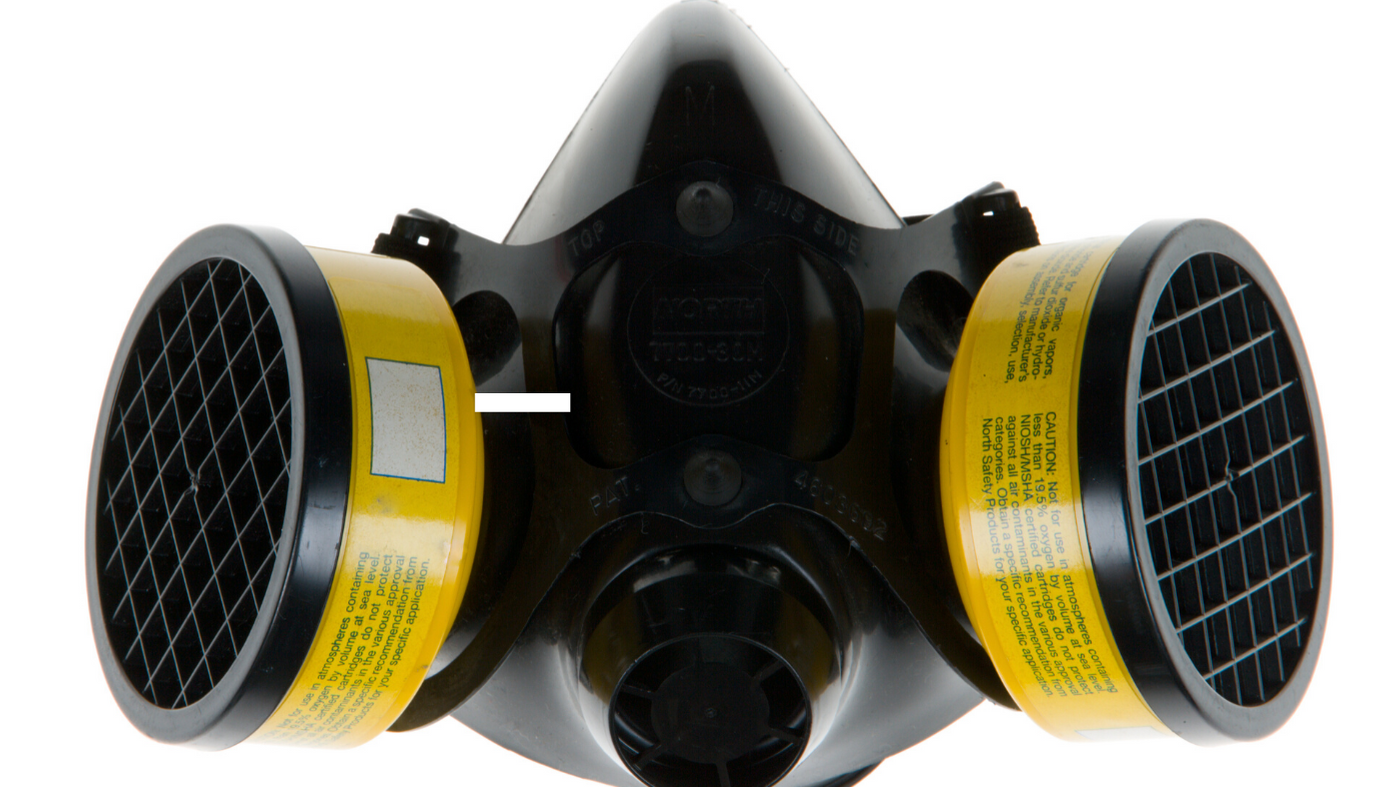
The pressure to purchase PPE without more consideration also puts patients at risk. Some dental offices fortunately purchased legitimate PPE, valved N95 masks and half-mask respirators. But unfortunately for patients, valved face coverings put patients at risk of infection from their providers.
Dentists have wasted thousands of dollars on potentially defective PPE or useless equipment. They struggled with the dilemma to find the globally recommended PPE or to see patients in much need after weeks of dental office closures.
To make matters worse, for almost the entirety in May, the American Dental Hygienists’ Association (ADHA) protested against opening dental offices to elective procedures. The ADHA’s strong position, which coincides with the CDC at the time, placed considerable tension between dental hygienists and dentists.
The heavy focus on PPE and AGPs also distracts dental personnel in conducting other effective transmission precautions, such as COVID-19 screening protocols and social distancing within the dental office.
POTENTIAL SOLUTIONS - Dentistry cannot forget the reason for its existence—providing oral health care for patients.
Although not ideal, doctors and nurses continued to see patients with or without proper PPE during the heat of the pandemic. It is one thing for healthcare personnel to advocate for more PPE during crises and shortages, but it is another to not treat at all due to their PPE, or lack thereof. Doctors and nurses are essential, and dentistry should be as well.
Concerns over a novel coronavirus and dental aerosol-generating procedures are not wrong. Keeping dental personnel and patients safe is extremely important to the community to curtail COVID-19.
But precautions in the dental office should not become so deliberating, and impossible, to prevent adequate dental patient care, especially with unproven effects of dental AGDs on COVID-19 transmission. Dental practices also are unlikely to treat actively sick patients, unlike healthcare workers on the frontlines.
Precautions for medical AGDs were based on studies from the first SARS outbreak in 2003-2004 where a few studies concluded that medical healthcare workers involving in AGDs contracted SARS. Even such research has been in debate as the etiology of airborne transmission could simply be from close contact with infected patients.
The CDC and OSHA need to find more dental collaborators, especially ones with current clinical experience, to assist in their guidelines and not just repurpose recommendations from medicine.
As experts in dentistry, the ADA can also exhibit more confidence in their recommendations and not defer so much to federal agencies. The ADA recognized the importance of continual dental treatment since the beginning of the pandemic but lacked the conviction to give non-ideal, alternative practice recommendations outside of CDC and OSHA guidelines.
One representation of the hierarchy of occupational hazard controls from the CDC.
In addition to a more patient-focused re-opening, dentistry should, instead, focus on other aspects of the hierarchy of infection controls, not just PPE.
Dentistry should focus on the elimination of the current work hazard—the most effective level in the hierarchy—and help advocate for more testing and contact tracing for COVID-19. With more data and mitigation efforts, dental personnel seeing COVID-19 positive patients would be even more unlikely, including pre-symptomatic patients.
Practice solutions and alternatives to PPE shortages need to exist for dental practices. “N95 masks or bust” should not be the motto of patient dental care.
In the end, the feedback loop amongst federal agencies, dental organizations, and dental providers over AGPs had good intent. But it can be broken and be replaced with more practical solutions for the dental community and its patients during these difficult times.





